Key Points
- Women are two times more likely than men to have IBS, with hormone changes playing a big part in how bad the symptoms are, especially during their period and menopause.
- Differences in female anatomy like the structure of the pelvic floor and slower movement in the gut help explain why more women have IBS where constipation is the main symptom.
- Hormone changes can affect how the gut moves, with high levels of estrogen and progesterone often slowing down digestion and making the intestines more sensitive to pain.
- Testing your gut bacteria with HerBiome Gut & Hormone Testing can give women specific information about how their gut health affects their hormone balance and IBS symptoms.
- Treatments for women with IBS should be tailored to their hormone cycles, with different plans needed during different times in their life from their period through menopause.
IBS affects up to 20% of Americans, but it hits women almost twice as often as men. This isn’t just a coincidence – there are certain biological, hormone, and even social reasons that make women more likely to get it. Knowing these female-specific causes is key to getting the right diagnosis and treatment.
Many women suffering from IBS struggle for years before receiving the care they need, often being told their symptoms are simply due to “stress” or are a “normal part of being a woman.” The truth is much more complicated, with female hormones, anatomy, and differences in the nervous system all playing major roles in the development of symptoms. AIMLabs’ HerBiome Gut & Hormone Testing provides women with a way to discover how their unique gut microbiome may be affecting their IBS symptoms and hormone health – an especially valuable tool considering how closely these systems are connected in the female body.
Why Women are More Prone to IBS than Men
It’s a fact: women are about twice as likely to develop irritable bowel syndrome as men. This isn’t a coincidence, but rather a reflection of the basic differences in female physiology, hormonal cycles, and even the way women’s pain is viewed by healthcare providers. Research consistently indicates that women experience more frequent and intense symptoms, especially constipation, bloating, and stomach pain.
Women’s symptoms also tend to follow more predictable patterns that correlate with hormonal fluctuations throughout the month. This is not coincidental – it’s direct evidence of how deeply interconnected the female reproductive and digestive systems truly are. During specific phases of the menstrual cycle, particularly around menstruation, up to 50% of women with IBS report worsened symptoms.
Moreover, women encounter specific health care difficulties when attempting to get a diagnosis and treatment. Studies indicate that women have to wait longer for GI referrals and their pain is often not taken as seriously as men who report the same symptoms. This delay in diagnosis means that women often endure more before they receive the proper care and management strategies.
Women’s Bodies: The Role of Hormones in IBS Symptoms
Women’s hormonal makeup sets the stage for IBS. Women, unlike men, undergo major hormonal changes throughout their menstrual cycle and at various points in their lives. These hormones don’t just impact reproductive organs – they have receptors all over the digestive tract that affect everything from gut movement to pain sensitivity.
The Impact of Estrogen and Progesterone on Digestive Function
The intricate interplay of estrogen and progesterone directly influences digestive function. When estrogen levels peak, as they do just before ovulation, it usually speeds up gut motility. Progesterone, on the other hand, which increases after ovulation, has the opposite effect – it slows down digestive transit and can potentially exacerbate constipation. This is why many women with IBS-C (constipation-predominant IBS) find their symptoms worsen during the luteal phase of their cycle.
These hormones can also influence gut permeability or how easily substances can pass through the intestinal wall. Higher estrogen levels can make the intestines more permeable, which may allow more irritants to pass through, leading to inflammation and sensitivity. This could explain why some women become more sensitive to certain foods at specific times during their menstrual cycle.
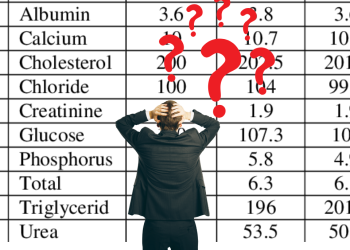
How Female Sex Hormones Affect IBS Symptoms
Estrogen: Can increase gut motility, enhance pain sensitivity, and increase intestinal permeability
Progesterone: Typically slows digestive transit, relaxes smooth muscle, and can worsen constipation
Monthly fluctuations: Create cyclical pattern of symptom severity that many women can track alongside their menstrual cycle
Menstrual Cycle Fluctuations and IBS Flares
The relationship between the menstrual cycle and IBS symptoms is so consistent that many gastroenterologists now recommend women track their symptoms alongside their cycle. During menstruation, when both estrogen and progesterone levels drop, many women experience their worst IBS symptoms – particularly increased pain sensitivity and changes in stool consistency. This isn’t psychosomatic; it’s a direct physiological response to changing hormone levels.
Prostaglandins, the compounds that are released during menstruation and cause the uterus to contract, also have an effect on the intestines that are nearby. These compounds can cause the gut to contract more, which can lead to cramping, urgency, and diarrhea in some women who have IBS. The combination of the shifts in hormones and the release of prostaglandins can create the perfect conditions for digestive problems to occur during the menstrual period.
Perimenopause and Menopause: Fluctuating Symptoms
Perimenopause and menopause are significant milestones in a woman’s life, and they can also mark a major shift in IBS symptoms. The hormonal changes that occur during perimenopause, which can start years before menopause, can cause IBS symptoms to become more erratic and harder to control. For some women, this means a marked increase in symptom severity, while others may notice their symptoms improving.
Research on the impact of menopause on IBS symptoms is mixed. A study by Lenhart et al. found that postmenopausal women with IBS often experience more severe symptoms than premenopausal women, suggesting that the sharp decrease in estrogen levels may have a lasting impact on gut function. However, other women find that their symptoms stabilize after menopause, potentially due to the end of cyclical hormone fluctuations. For more information on related topics, you might find this article on andropause and male menopause symptoms interesting.
Another factor that adds to the complexity is hormone replacement therapy (HRT). Some studies suggest that HRT may cause IBS symptoms in postmenopausal women who did not have symptoms before, while other studies suggest that the impact is minimal. This conflicting information highlights the importance of personalized treatment and the value of tests like HerBiome that can identify individual gut microbiome patterns that affect hormonal balance.
Do Birth Control Pills Help or Harm IBS?
For a lot of women, using hormonal contraceptives is a catch-22 when it comes to managing IBS. Some women say their symptoms improve a lot when they take birth control pills, probably because these pills keep hormone levels steady instead of letting them go up and down throughout the month. By stopping the big drops in estrogen and progesterone that happen when a woman has her period, these drugs can make IBS flare-ups less cyclical.
On the other hand, some women find that hormonal contraceptives actually make their digestive symptoms worse. This is probably due to individual differences in gut sensitivity and the way each woman’s body reacts to synthetic hormones. The type of birth control also makes a difference – pills with a higher dose of estrogen may have a different effect on gut function than low-dose or progesterone-only options.
How Female Anatomy Can Lead to a Higher Risk of IBS
Along with hormonal factors, the physical differences between men and women also contribute to the higher prevalence of IBS in women. Women’s digestive and pelvic organs are located closer together than men’s, which can lead to unique symptom patterns and risks. These anatomical differences help us understand why women are not only more likely to have IBS, but also why they often have different symptoms than men.
The Link Between IBS and the Anatomy of the Female Pelvic Floor
When compared to men, the anatomy of the female pelvic floor is more intricate. The digestive, reproductive, and urinary tracts are all located in close proximity to each other. This closeness can cause dysfunction in one system to impact the others, resulting in overlapping symptoms. Almost half of all women with IBS also experience urinary symptoms or pelvic pain – a trend that is less frequent in men.
Women’s pelvic floors also have to deal with the strains of pregnancy and childbirth, which can cause lasting changes to how the pelvic floor functions. Studies have found that women who have given birth naturally are more likely to suffer from pelvic floor dysfunction. This can cause or make IBS symptoms worse, particularly constipation and feeling like you haven’t fully emptied your bowels. This link could be why many women first start to experience IBS symptoms after giving birth.
Women’s Digestive Systems Process Food More Slowly
Food generally takes longer to pass through a woman’s digestive system than a man’s, with an average transit time through the colon that is 14 hours longer. This slower processing time is one reason why IBS-C (constipation-predominant) is more prevalent in women, while men are more likely to have IBS-D (diarrhea-predominant) patterns. Furthermore, the female colon has more serotonin receptors than the male colon, resulting in varying sensitivity to pain and motility signals.
What this means is that treatments that work for men may not work as well for women. Certain medications, for example, may affect men and women differently due to the way they target serotonin receptors. That’s why it’s important to use testing approaches like HerBiome that take these biological differences into account. This can help us identify more effective treatment strategies that are specifically tailored to women.
Differences in the Brain-Gut Connection Between Genders
Significant gender-based differences have been found in the brain-gut axis, which is the communication pathway between the central nervous system and the digestive tract. Neuroimaging studies have shown that women process visceral pain differently than men, with more activation in the emotional centers of the brain. This is why women often have more intense emotional components to their IBS symptoms, including anxiety about symptoms and anticipatory stress.
Women also demonstrate different patterns of central pain processing, with increased sensitivity to repeated painful stimuli. This “central sensitization” implies that women may develop more persistent and widespread pain responses to gut irritation. This neurological difference isn’t psychological – it’s a biological fact that impacts how women experience IBS symptoms and respond to treatments targeting pain perception.
Mental Health and IBS in Women
IBS is primarily a gut-brain interaction disorder with biological roots, but mental health also plays a significant role, particularly in women. The two-way communication between the brain and the gut means that emotional states can initiate or exacerbate symptoms, while ongoing digestive symptoms can impact mental health. Recognizing these links is key to a holistic treatment approach.
The Digestive Effects of Stress Response
Women have a unique response to stress compared to men, which includes specific patterns of hormone release and nervous system activation. When confronted with stress, women exhibit a higher activation of the hypothalamic-pituitary-adrenal axis, which impacts gut function through stress hormones such as cortisol. These hormones directly influence gut motility, secretion, and intestinal permeability – all of which are critical factors in the development of IBS symptoms.
Moreover, women’s bodies usually hold onto stress hormones for longer periods of time after a stressful event than men. This extended stress response can result in ongoing digestive symptoms even after the initial stressor is no longer present. The stress response in women also shows a greater involvement of immune system activation, which may contribute to the heightened inflammation often seen in many women with IBS.
Why Women with IBS Often Have Anxiety and Depression
Women who have IBS often have anxiety and depression too, more so than men who have IBS. While these mental health conditions don’t cause IBS, they are related in a complex way to digestive symptoms, and can make each other worse. The neurotransmitters that help regulate mood, especially serotonin, also help the gut function properly. This creates biological pathways that allow emotional states to affect digestive symptoms.
Women are generally more likely to suffer from anxiety disorders than men, with about twice as many women affected. This makes them more susceptible to an increase in symptoms. Studies have shown that anxiety specifically increases the sensitivity of gut pain and changes the movement patterns in a way that can trigger or worsen IBS symptoms. This connection helps to explain why treatments that address both psychological and digestive symptoms often provide better results for women with IBS.
How Trauma History Influences IBS Development
There is a strong correlation between a history of trauma, especially abuse, and the development of IBS, and this link is notably more prevalent in women than in men. Research consistently indicates that women who have experienced physical, sexual, or emotional abuse are significantly more likely to be diagnosed with IBS. This relationship seems to be due to enduring changes in the communication pathways between the gut and the brain, with early trauma causing irreversible changes in the body’s processing and response to gut sensations. For more insights on prioritizing mental health, consider breaking the stigma around mental health care.
The link between trauma and IBS is not just psychological – it causes real, quantifiable changes in how the gut functions, how pain is processed, and how the body responds to stress. Recognizing this connection is vital for creating treatment strategies that are compassionate and effective, treating the person as a whole rather than just managing their physical symptoms. For many women, strategies for care that are informed by trauma and that create a sense of safety and control can be especially helpful for managing IBS symptoms.
Obstacles in Social and Healthcare Women Encounter
In addition to biological elements, women suffering from IBS must deal with considerable social and healthcare hurdles that can postpone diagnosis and appropriate treatment. The path to successful IBS management is typically longer and more exasperating for women, who often confront doubt or disregard of their symptoms. These obstacles are a vital part of the female IBS experience that affects both physical health and life quality.
How Gender Influences Digestive Health Diagnosis
Studies have consistently found that gender plays a significant role in how digestive health issues are diagnosed and treated. Women generally have to wait longer to be referred to a gastroenterology specialist, are less likely to undergo diagnostic procedures, and are more likely to be given psychological explanations for their symptoms than men. This delay in diagnosis and treatment means women often endure their symptoms for a longer period of time and their symptoms may become more severe before they receive the appropriate treatment.
Women’s physical symptoms are often attributed to emotional causes, which can make diagnosing IBS particularly difficult. The gut-brain connection is crucial for all IBS patients, but women’s symptoms are often dismissed as “just stress” or “anxiety” before a comprehensive physical evaluation is done. This bias can result in missed diagnoses of other conditions that frequently overlap with or mimic IBS, such as endometriosis, inflammatory bowel disease, or celiac disease.
Dismissal as “Just Stress”
Women who have IBS often hear that their symptoms are all in their heads, not in their bodies, which can be particularly vexing given the clear physical causes of the disorder. This dismissive attitude can lead to treatments that only focus on the mental aspects, ignoring the very real physical aspects of IBS that need medical treatment. For a deeper understanding of how physical symptoms can be misinterpreted, you might explore resources on DNA testing and health.
The “it’s all in your head” dismissal not only adds an extra psychological burden, but it also causes women to start doubting their own experiences and possibly delay seeking further care. Studies have shown that women who are dismissed in this way often develop increased anxiety about their symptoms and are more reluctant to discuss them with healthcare providers – creating a dangerous cycle that further delays the right diagnosis and treatment.
Dismissing Women’s Symptoms
When women report IBS symptoms, they are often dismissed, especially when they coincide with their periods. Symptoms that greatly affect their quality of life are often dismissed as “normal” period complaints, rather than recognized as part of a chronic digestive condition that needs specific treatment. This dismissal leads many women to normalize their own pain, accepting severe symptoms as an inevitable part of being a woman.
There’s a surprising lack of focus on the connection between female hormones and digestion in healthcare education. This has resulted in a knowledge gap that has a direct impact on clinical practice. Many healthcare providers have received little to no training on how to assess and treat the symptoms of gynecological and digestive conditions that overlap. This leaves women who have complex symptom patterns at risk of receiving care that only addresses part of their symptoms.
Distinct IBS Symptoms in Women
Although IBS symptoms are the same in both men and women, women often experience unique symptom patterns that are influenced by their unique physiology. Recognizing these female-specific symptoms helps patients and healthcare providers accurately identify IBS and create effective treatment plans. These differences aren’t just statistical, they represent fundamental biological differences in how IBS presents itself in women.
Why Women are More Likely to Experience IBS-C
Women are more likely to experience constipation-predominant IBS (IBS-C) than men. Studies show that nearly 60% of women with IBS primarily experience constipation, compared to about 30% of men. This disparity is due to both hormonal and anatomical factors. The hormone progesterone naturally relaxes smooth muscle, including the muscles in the intestines. This contributes to slower transit time in women, especially during the luteal phase of the menstrual cycle when progesterone levels are at their highest.
Women’s unique pelvic floor structure is another factor that leads to higher rates of constipation. The female pelvic floor has to accommodate multiple organ systems in a small space, which can lead to coordination problems during bowel movements. Pregnancy and childbirth can also permanently change how the pelvic floor functions, increasing the risk of constipation. This is why many women start experiencing symptoms of IBS-C after they have children.
Bloating: The Number One Complaint Among Women
For women, bloating is the most frequently reported and often the most troubling symptom of IBS. Research indicates that as many as 96% of women with IBS regularly experience bloating, compared to roughly 60% of men with the disorder. This bloating usually follows a cyclical pattern that becomes more severe during the luteal phase and early menstruation, when hormonal changes naturally cause an increase in fluid retention and gas production. For more insights into how hormonal changes affect women, you can explore this guide on symptoms and treatments of hormonal shifts.
Women’s unique abdominal and pelvic structures may make bloating more noticeable and uncomfortable. Women’s abdominal organs are closer together in a smaller space, so there’s less room to stretch when gas or fluid levels rise. Women also seem to be more sensitive to normal amounts of intestinal gas, feeling discomfort at volumes that usually don’t cause symptoms in men.
Most Common IBS Symptoms in Women (Ranked by Frequency)
1. Abdominal bloating (up to 96% of women with IBS)
2. Abdominal pain/discomfort (80-90%)
3. Constipation (60-70%)
4. Fatigue (60-70%)
5. Sleep disturbances (30-50%)
6. Diarrhea (30-40%)
7. Nausea (30-40%)
Pain Perception Differences Between Men and Women
Women generally perceive visceral pain more intensely than men, with lower pain thresholds and greater pain sensitivity in the digestive tract. This isn’t psychological – it reflects actual differences in pain processing pathways, with women showing more activation in brain regions involved in pain amplification and emotional processing. These biological differences help explain why women with IBS typically report more severe and widespread pain than men with identical objective findings.
Changes in hormone levels also affect how sensitive a woman is to pain. Many women feel pain more intensely during the late luteal phase and menstruation, when their estrogen and progesterone levels are lower. This hormonal effect on how pain is processed can create patterns of symptom intensity that many women can track along with their menstrual cycles. Knowing these patterns can allow for treatments to be timed more strategically to address symptom flares that can be predicted.
5 Treatment Approaches That Work Best for Women
Effective IBS management for women requires approaches that acknowledge female-specific factors affecting symptoms. Rather than generic treatments, women often benefit most from strategies that account for hormonal fluctuations, anatomical considerations, and women’s unique pain processing patterns. These targeted approaches offer greater symptom relief by addressing the root causes of female IBS manifestation.
1. Dietary Changes That Take Hormones Into Account
Dietary management is a key part of treating IBS, but women get the most benefit from methods that take into account the cyclical changes in hormones. Low-FODMAP diets, which limit fermentable carbohydrates that can set off symptoms, might need to be changed during different parts of the menstrual cycle. Many women find that they can handle FODMAPs better during the follicular phase when estrogen is more prominent, while they need to stick more closely to the diet during the luteal phase when progesterone increases.
Strategic timing of fiber intake based on hormonal status can also benefit women. Soluble fiber generally helps regulate bowel function throughout the month, but insoluble fiber may be better tolerated when estrogen levels are high and constipation is less likely. Eating small, frequent meals rather than large ones can help minimize the effects of hormonal fluctuations on the time it takes for food to pass through the digestive system, providing more consistent symptom management throughout the menstrual cycle.
2. Managing IBS with Cycle-Syncing
For women who suffer from IBS, cycle-syncing, or adapting treatments and self-care practices to fit with the phases of the menstrual cycle, can be a game-changer. This approach acknowledges the fact that symptoms often follow patterns that can be predicted, which are in line with hormonal fluctuations. During the follicular phase, which spans days 1-14, estrogen levels rise and progesterone levels remain low. Many women find that their IBS symptoms lessen during this phase and that they can eat a wider variety of foods. The luteal phase, which spans days 15-28, often brings with it an increase in bloating, constipation, and pain sensitivity as progesterone levels rise. This phase often requires more aggressive strategies for managing symptoms and stricter adherence to dietary restrictions.
3. Pelvic Floor Physiotherapy
Many women with IBS have pelvic floor dysfunction, which plays a significant role in their symptoms. This is why pelvic floor physiotherapy is a crucial treatment for many women with IBS. Pelvic floor physiotherapists who are trained can identify and treat issues with muscle coordination, tension patterns, and weakness that affect both bowel function and pain. Research has shown that women with IBS who have pelvic floor physiotherapy see a significant improvement in their constipation, incomplete bowel movements, and pain. They often see better results than if they were only using medication.
4. Proven Results of Mind-Body Techniques
Mind-Body Therapies for Women with IBS and Their Effectiveness
Gut-directed hypnotherapy: 70-80% symptom improvement
Cognitive behavioral therapy: 60-70% symptom improvement
Mindfulness-based stress reduction: 30-50% symptom improvement
Yoga (IBS-specific protocols): 30-40% symptom improvement
Source: Systematic review of 20+ randomized controlled trials, with female patients showing stronger response than male patients across all techniques
Mind-body techniques are especially effective for women suffering from IBS, probably due to the stronger gut-brain connection seen in female patients. Gut-directed hypnotherapy, which employs guided imagery specifically aimed at normalizing digestive function, is one of the most strongly supported treatments. Clinical trials have shown that it reduces IBS symptoms in women by 70-80% when a full treatment protocol is completed, with benefits lasting for years after the end of treatment.
Customized cognitive behavioral therapy (CBT) for IBS not only addresses the mental aspects of the disorder but also helps create targeted coping mechanisms for managing symptoms. Women generally have a more robust response to CBT than men, likely because the treatment directly tackles catastrophizing and anxiety – elements that usually have a more significant impact on women’s symptom experience.
Many women with IBS experience a cycle of anxiety and pain. Mindfulness practices that focus on being aware of the present moment without judgment can help to break this cycle. Regular mindfulness practice can actually change how the brain processes pain, reducing the emotional amplification of digestive discomfort. Even short daily mindfulness exercises have been shown to reduce the severity and frequency of symptoms in women with IBS.
5. Medications Specifically Designed for Women
When it comes to treating IBS in women, the medication approach often needs to be tailored specifically for them. This includes adjusting for different phases of the menstrual cycle and understanding how sex hormones can affect the way drugs are metabolized. Some medications, like certain serotonin modulators, are more effective in women, while others may need to be adjusted in dosage throughout the menstrual cycle. Women also metabolize many IBS medications differently than men, sometimes requiring lower starting doses to avoid side effects while still getting relief from symptoms. Testing solutions like HerBiome can help identify which gut microbiome patterns may affect how a woman responds to specific IBS medications, allowing for more personalized treatment selection.
Manage Your IBS Effectively
For women who suffer from IBS, it’s essential to understand the unique factors that can impact your symptoms and to take a proactive approach to managing your condition. Keep track of your symptoms in relation to your menstrual cycle to see if there are any patterns, and don’t be afraid to seek out healthcare providers who have a good understanding of the factors specific to women’s IBS. You might also want to consider undergoing comprehensive tests like HerBiome, which can help to establish the link between your gut microbiome and your hormonal health. This can provide you with insights that are specific to the female body and the complex interactions between the digestive and reproductive systems.
Don’t forget that managing IBS often requires a combination of various methods – changes in diet, stress management, perhaps medication, and dealing with any pelvic floor dysfunction. The aim is not just to reduce symptoms but to restore your quality of life and confidence in your body’s performance. With targeted approaches specific to women, most women with IBS can experience a significant improvement in symptoms and return to the activities they enjoy.
Common Questions
A lot of women who have IBS wonder how it affects their unique life experiences and biological processes. These common questions address some of the most frequent worries and give answers based on research to help women understand and manage their symptoms in different life stages and situations.
Does pregnancy worsen IBS symptoms?
IBS symptoms during pregnancy vary from woman to woman, with about 40% seeing an improvement, 35% experiencing worsening symptoms, and 25% reporting no significant change. During the first trimester, increased progesterone levels often make constipation and bloating worse. However, as the pregnancy progresses, many women find their IBS symptoms actually get better. This could be due to the anti-inflammatory effects of certain hormones released during pregnancy or changes in the immune system that reduce gut sensitivity.
Managing IBS During Pregnancy: Safety Considerations
Safe: Dietary management, approved probiotics, gentle fiber supplements, physical activity, mind-body techniques
Use with medical supervision only: Antispasmodics, certain laxatives, specific anti-diarrheal medications
Typically avoided: Eluxadoline, alosetron, most antidepressants used for IBS, rifaximin
The pressure of the growing uterus on intestinal organs can create mechanical changes that affect symptom patterns, particularly in the third trimester. Constipation often worsens late in pregnancy due to this pressure combined with slowed intestinal transit time. However, some women with diarrhea-predominant IBS find this pressure actually helps regulate their bowel movements.
During pregnancy, it’s crucial to carefully consider treatment options to ensure the safety of both mother and child. Most standard IBS medications are not recommended during pregnancy, making lifestyle changes like diet, gentle exercise, and stress reduction crucial. Collaborating with healthcare providers who are knowledgeable about both IBS and prenatal care is vital for creating safe and effective strategies for managing symptoms.
Should women with IBS avoid specific foods during their period?
Many women with IBS find that avoiding certain trigger foods during menstruation helps reduce hormone-driven symptoms. High-FODMAP fruits and vegetables like apples, pears, and cauliflower can cause increased bloating during this time when the body is already more likely to retain fluid. Foods that cause inflammation, such as processed meats, fried foods, and too much sugar, can make period-related discomfort and IBS pain worse.
Women with IBS should be especially mindful of their caffeine and alcohol consumption during their period. Both can heighten the sensitivity and motility of the intestines, which could amplify cramps and diarrhea. A number of women have found that cutting their caffeine intake in half during their period can help to control both digestive and menstrual symptoms.
Many women find that dairy products impact them differently during their period because of temporary shifts in lactase enzyme production. Even women who usually tolerate some dairy may find that they’re more sensitive during their period. Lactose-free alternatives or plant-based options often offer better tolerance during this time.
Instead of solely concentrating on what to avoid, it can be helpful to focus on what to eat to manage both IBS and menstrual symptoms. Foods high in magnesium, such as dark leafy greens and pumpkin seeds, may help alleviate menstrual cramps and IBS pain. Anti-inflammatory foods like fatty fish, turmeric, and ginger can help control the inflammation that contributes to both sets of symptoms. For more insights on managing health through diet, check out these tips on managing blood sugar spikes.
Recommended Foods During Menstruation for Women with IBS
– Low-FODMAP fruits: bananas, blueberries, grapes, oranges, strawberries
– Easily digestible proteins: well-cooked eggs, tofu, plain chicken
– Anti-inflammatory options: fatty fish, turmeric, ginger tea
– Soothing carbohydrates: white rice, oatmeal (if tolerated), sourdough bread
– Magnesium-rich foods: spinach, pumpkin seeds, dark chocolate (in moderation)
Does hormone replacement therapy help or worsen IBS symptoms?
The relationship between hormone replacement therapy (HRT) and IBS symptoms presents a complex picture with significant individual variation. Research shows conflicting results – some studies suggest HRT may trigger or worsen IBS symptoms in postmenopausal women, while others indicate potential benefits for certain symptom patterns. A 2003 study by Ruigomez found that postmenopausal women starting HRT had a slightly higher risk of developing IBS than those not using hormonal treatments, suggesting that introducing external hormones may disrupt established digestive patterns.
The exact type of HRT you use can affect the outcome. It seems that estrogen-only formulas are less likely to make IBS symptoms worse than combined estrogen-progesterone treatments. This makes sense when you consider that progesterone can slow down the time it takes for food to move through your intestines, which can make symptoms of IBS with constipation worse. So, women with IBS-C may have more severe digestive side effects from combined HRT than those with IBS-D.
How HRT Affects IBS Based on Symptom Type
IBS-C (Constipation predominant): Combined HRT often makes symptoms worse, but estrogen-only formulations might help
IBS-D (Diarrhea predominant): Combined HRT sometimes helps, but responses to estrogen-only are inconsistent
IBS-M (Mixed type): Responses are highly variable and depend on the individual
Source: Analysis of data from the Women’s Health Initiative and other long-term studies
The decision to use HRT should take into account how it might affect IBS, as well as other health factors and quality of life considerations. For women who have severe menopausal symptoms and IBS, the benefits of HRT might outweigh the potential negative effects on digestion. It’s important to closely monitor symptoms and be willing to adjust treatment approaches based on how an individual responds. Testing through platforms like HerBiome can provide insights into how a woman’s gut microbiome might interact with hormone treatments, which can help predict how an individual will respond to HRT.
Why do some women report improvement in IBS symptoms after menopause?
About 30-40% of women have reported that their IBS symptoms improved after they reached menopause, especially those who previously had clear cyclical patterns associated with their menstrual cycle. This improvement is likely due to the stabilization of sex hormones at consistently lower levels, which eliminates the dramatic fluctuations that triggered symptoms during reproductive years. For women whose IBS symptoms were mainly caused by hormonal changes rather than other factors, this stabilization can provide significant and lasting relief from the cyclical pattern of flares they experienced for decades. For more information on hormonal changes, you can refer to this article on pheromones and hormones.
Is stress management the key to reducing IBS symptoms in women?
While stress management can help reduce IBS symptoms in many women, it is not a cure-all. Clinical studies have found that dedicated stress reduction programs can reduce symptom severity by 30-50% in women with IBS. This includes improvements in pain, bloating, and emotional well-being. Women often respond better to stress management interventions than men. This is likely due to the way stress impacts the female digestive system through both the nervous system and hormonal pathways.
Stress management effectiveness is dependent on individual symptom patterns and triggers. Women who primarily have symptoms triggered or worsened by stress often see the most significant improvements. Those with mainly physiological triggers may see more modest benefits, but still a significant improvement in their overall symptom management and quality of life.